The eye offers opportunities to capture critical information regarding the health of the brain, as the neurological anatomy and the microvasculature of the retina are very closely related to those of the brain and can be similarly affected by certain pathological processes. In this study published in the Journal of Alzheimer's Disease, Dr. Cecilia Lee and her co-authors compared brain neuropathology findings with known clinical information to determine if there were any associations between certain eye diseases and the presence of characteristic neuropathologic lesions of Alzheimer's disease. The authors analyzed the data from 676 patients from Adult Changes in Thought, a prospective longitudinal study in older patients who are followed over time and monitored for development of cognitive decline and dementia.
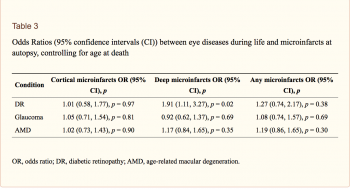
The authors previously found that diabetic retinopathy, glaucoma, and age-related macular degeneration, all neurodegenerative diseases of the eye, were each significantly associated with development of clinical Alzheimer's disease. In this study, the authors examined various neuropathological findings associated with Alzheimer's disease, including Braak stage and CERAD score (measures of neurofibrillary tangles and amyloid plaques, respectively), Lewy bodies, hippocampal sclerosis, microvascular brain injury, and quantitative paired helical filament (PHF)-tau levels. They compared these findings in people with and without each eye disease to determine if there were any correlations.
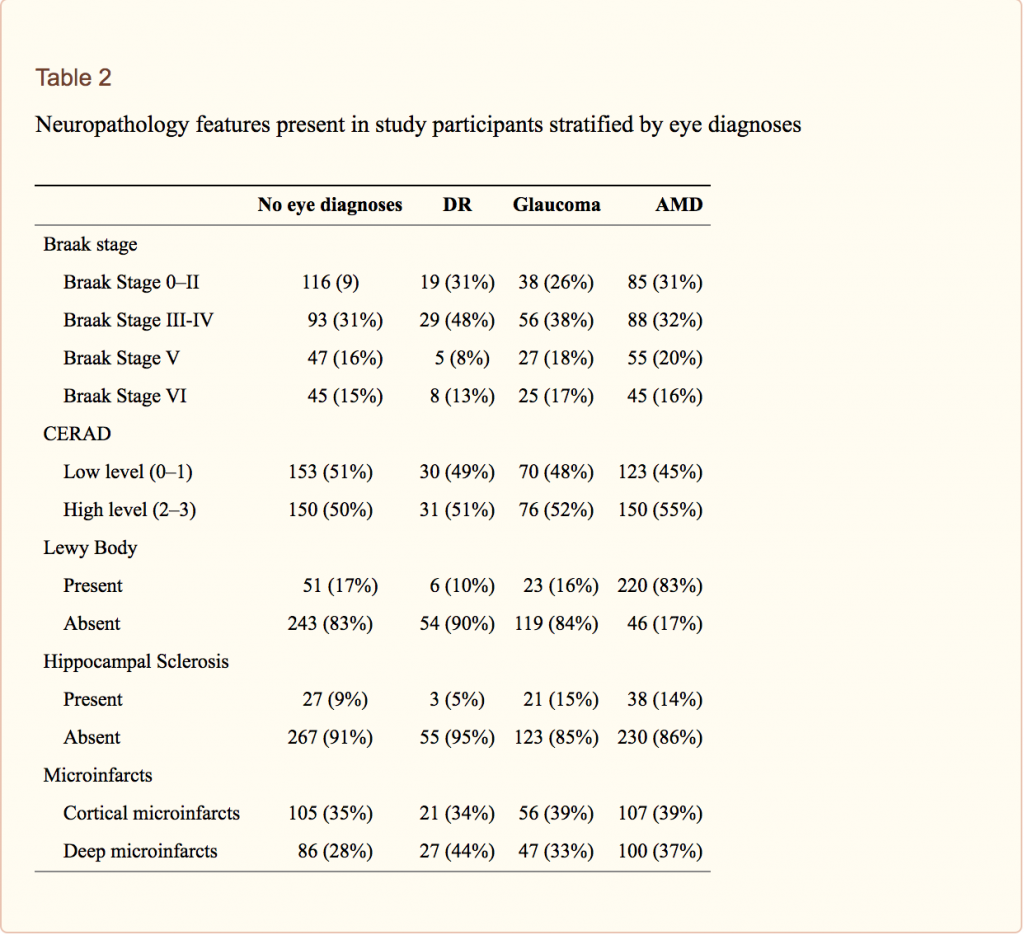
They found a strong association between diabetic retinopathy and the risk of deep microinfarcts in the brain. One theory that may explain this finding is that that the loss of endothelial pericytes in the retina is believed to be the initiating pathology of diabetic retinopathy, and similar loss of endothelial integrity of the brain microvasculature may also take place in patients with diabetic retinopathy. This finding could be useful clinically because dilated funduscopic examination is noninvasive and could potentially be used as a screening tool to identify patients who are more likely to have microvascular brain injury. The authors note, however, that cortical microinfarcts, rather than deeper subcortical microinfarcts, are more associated with dementia risk.
Higher amounts of PHF-tau were associated with glaucoma, with an increased trend for pathological tau in the occipital cortex, although it did not reach statistical significance. The authors hypothesized that the loss of retina ganglion cells in glaucoma may influence cerebral cortical (occipital) PHF-tau deposition because the afferent input from these cells may have served a protective role against tau pathology in the occipital cortex.
Further studies are warranted to investigate these potential connections between neurodegenerative diseases of the eye and Alzheimer's disease, with the hope of finding noninvasive methods of eye examination that may provide useful information about neurodegenerative processes in the brain.
Lee CS, Larson EB, Gibbons LE, Latimer CS, Rose SE, Hellstern LL, Keene CD, Crane PK. Ophthalmology-Based Neuropathology Risk Factors: Diabetic Retinopathy is Associated with Deep Microinfarcts in a Community-Based Autopsy Study. J Alzheimers Dis. 2019;68(2):647-655. doi: 10.3233/JAD-181087. PubMed PMID: 30883356; PubMed Central PMCID: PMC6450649.