The purpose of this interesting study by Dr. Lee and her co-authors was to better understand how ophthalmologists order tests when evaluating patients with uveitis. There are about 150,000 cases of uveitis (inflammation of the uvea) in the United States each year, and testing for treatable diseases as well as other health issues that might be associated with uveitis is an important part of the workup when patients present with this condition. However, unlike many other ophthalmic conditions, there is no "standard laboratory workup" for uveitis, and unfocused ordering of diagnostic tests can be difficult to interpret and costly.
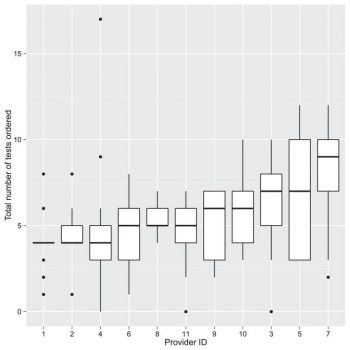
The authors created web-based survey with thirteen hypothetical clinical scenarios of real-life diagnostic challenges. Eleven practicing uveitis specialists completed the survey, in which they were asked to list the investigations that they would order for each scenario. The ophthalmologists who completed the survey included a mix of hospital-based and outpatient-based clinicians. In all, they ordered a total of 782 investigations for the 13 scenarios, including forty-five different tests (laboratory tests as well as imaging and diagnostic procedures). The mean number of tests ordered per scenario per provider was 5.47 +/- 2.71, and the mean cost per scenario per provider was $282.80 (range $0 to $1145.50). There was limited agreement between the physicians about which tests to order for each scenario. They reached universal agreement on only one test (antineutrophil cytoplasmic antibody) for 1 scenario (Scenario 9, unilateral scleritis). Most laboratory tests were ordered by less than half of the participants.
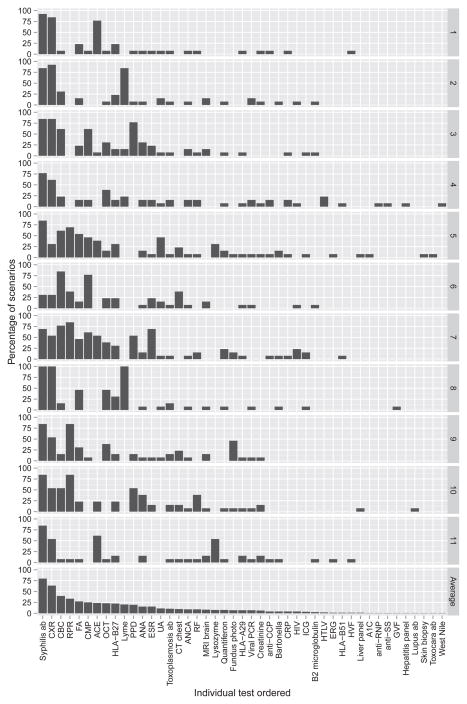
Based on these results, the authors conclude that consensus between uveitis experts on which tests are needed remains low, although they note that the survey was given to only a small subset of uveitis subspecialist ophthalmologists, and that the scenarios are likely not as informative as actual patient encounters. However, the authors conclude that the wide variability in testing approaches suggests the lack of an evidence-based diagnostic approach. They recommend that a consensus expert panel develop a set of recommendations that could help guide clinicians when making decisions about how to evaluate a patient with uveitis.
Lee CS, Randhawa S, Lee AY, Lam DL, Van Gelder RN. Patterns of Laboratory Testing Utilization Among Uveitis Specialists. Am J Ophthalmol. 2016 Oct;170:161-167. doi: 10.1016/j.ajo.2016.08.004. Epub 2016 Aug 10. PubMed PMID: 27521608; PubMed Central PMCID: PMC5056154