In this large, national, multicenter study, the authors evaluated two drugs used to treat age-related macular degeneration, the leading cause of blindness in adults over 50 in the United States. The drugs, ranibizumab and aflibercept, are vascular endothelial growth factor inhibitors, and both are used to slow disease progression (and vision loss) by preventing choroidal neovascularization.
One known problem with these drugs is tachyphylaxis, or a weakening in response to the drug due to long-term or repeated exposure. Because of tachyphylaxis, clinicians sometimes change to a different drug hoping for a better effect, and the authors were interested in whether or not this strategy actually improved outcomes for patients. For a long time in the United Kingdom, ranibizumab was the only vascular endothelial growth factor inhibitor available through the National Health Service for treating age-related macular degeneration. When aflibercept became available, many patients in the UK switched from ranibizumab to aflibercept, which created a perfect population in which to study the effects of changing to a different drug after long term treatment with a vascular endothelial growth factor.
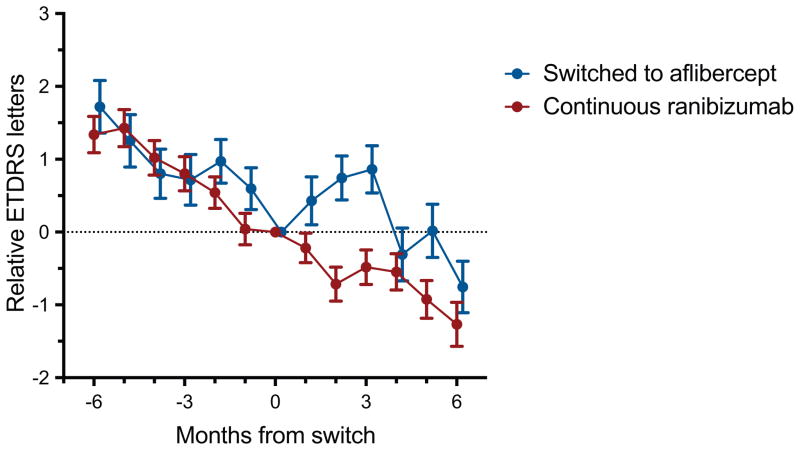
Change in visual acuity. The graph illustrates a comparison of visual acuity (relative Early Treatment Diabetic Retinopathy Study (ETDRS) letters) over time (months) between the switch group and the continuous ranibizumab group. Negative months indicate time before the switch. Error bars (± SD).
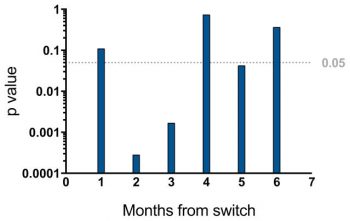
The authors looked at the visual acuity measurements of 448 patients who switched from ranibizumab to aflibercept and compared their outcomes to 896 patients who continued taking ranibizumab. They found that the patients who changed therapies showed improvements in visual acuity at 2, 3, and 5 months after the switch, but these visual acuity gains started to decline around 4 to 6 months after the change in a way that was similar to the control group.
The authors explore various explanations for this observation, including whether the newer drug (aflibercept) may be more effective or whether the improvements in visual acuity occured after switching drugs because of tachyphylaxis. Because of its large size, his study provided new insights into the long term effects of using these drugs that may help guide clinical decisions about their use. More studies are needed to further investigate the use of vascular endothelial growth factor inhibitors and tachyphylaxis, as well as the relative effectiveness of the available drugs.
Lee CS, Kim AJ, Baughman D, Egan C, Bailey C, Johnston RL, Natha S, Khan R, Brand C, Akerele T, McKibbin M, Downey L, Al-Husainy S, Lee AY, Tufail A. VISUAL ACUITY IMPROVEMENT WHEN SWITCHING FROM RANIBIZUMAB TO AFLIBERCEPT IS NOT SUSTAINED. Retina. 2018 May;38(5):951-956. doi: 10.1097/IAE.0000000000001637. PubMed PMID: 28406859; PubMed Central PMCID: PMC5636644.