In this multicenter study in the UK, the authors analyzed the electronic medical records of patients with age-related macular degeneration and compared two different drugs, ranibizumab and aflibercept, commonly used to treat this disease. Neovascular age-related macular degeneration is characterized by choroidal neovascularisation, which is responsible for the majority of visual loss. Intravitreal injections with vascular endothelial growth factor-A inhibitor drugs can reduce abnormal blood vessel growth and improve vision. This studied compared the effectiveness of two of these drugs, ranibizumab and aflibercept, by analyzing the visual acuity outcomes in patients who received either drug over a one year period.
Ranibizumab is typically given to patients in a schedule of three initial doses, followed by further doses as needed. The dosing schedule for aflibercept, a newer drug, is typically given in a fixed schedule (such as regular monthly doses) or using "treat and extend" protocol. With treat and extend, the patient receives regular treatments until the neovascularization is controlled, and then the time between treatments is gradually extended. The preferred treatment and dosing schedules for each drug used by the National Health Service in the UK provided excellent data for comparing these two drugs and their most common dosing regimens.
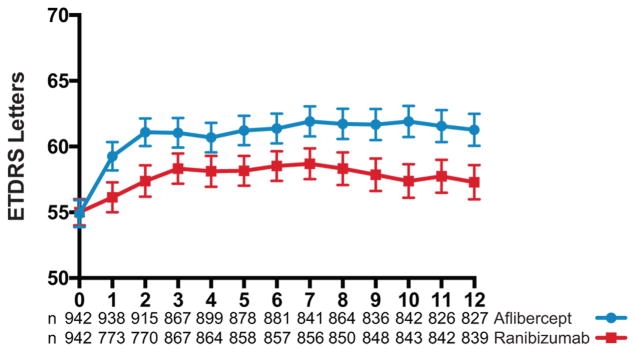
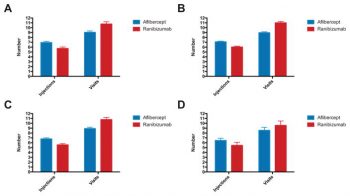
The authors looked at changes in visual acuity measurements to measure the effectiveness of the two treatments. They found that visual acuity was significantly higher in patients who had been treated with aflibercept (either with fixed dosing or with the treat and extend protocol) compared to patients who had received ranibizumab (three doses then as needed regimen) one year after the start of treatment. Overall, the patients on ranibizumab gained 1.6 letters on the eye chart, while patients on aflibercept gained 6.1 letters, and the difference was greatest in the patients that had the poorest visual acuity before treatment. Patients in the aflibercept group had more injections (mean=7.0 vs 5.8) but fewer clinic visits (mean=9.0 vs 10.9) than ranibizumab.
This was a significant finding, as this was a very large study reporting the real-world visual outcomes of patients on ranibizumab versus aflibercept therapy. The authors noted that the different outcomes for VA of the two drugs in this study could either be related to differences between the two drug's actions or due to the different delivery strategies. Other studies, however, have not found a significant differences in outcomes between these two drugs, and an early results from another study found that giving ranibizumab using the fixed or treat and extend dosing schedule may lead to better outcomes.
The authors conclude that the different dosing regimen is the most likely explanation for the different visual acuity outcomes with these two drugs, and that patients on as-needed ranibizumab therapy should consider shifting to a continuous (fixed, or treat and extend) dosing schedule.
Lee AY, Lee CS, Egan CA, Bailey C, Johnston RL, Natha S, Hamilton R, Khan R, Al-Husainy S, Brand C, Akerele T, Mckibbin M, Downey L, Tufail A. UK AMD/DR EMR REPORT IX: comparative effectiveness of predominantly as needed (PRN) ranibizumab versus continuous aflibercept in UK clinical practice. Br J Ophthalmol. 2017 Dec;101(12):1683-1688. doi: 10.1136/bjophthalmol-2016-309818. Epub 2017 May 6. PubMed PMID: 28478396; PubMed Central PMCID: PMC5673590.