In this large study using data from more than 30,000 patients in the UK, the authors analyzed potential risk factors for developing proliferative diabetic retinopathy and vitreous hemorrhage in patients with diabetes mellitus. Diabetic retinopathy is a major cause of blindness in working-age adults, and early detection can substantially decrease the risk of progression to vision loss. Patients with diabetes should have regular screening for early signs of diabetic retinopathy, but the current severity classification systems may not be the most accurate method for predicting which patients are most at risk for vision-threatening disease, particularly as standards of care have been updated.
The UK has a unique screening system in that each clinical feature of diabetic retinopathy is entered by physicians at baseline and at each retina clinic visit in a structured manner. The authors retrospectively analyzed this clinical data to determine current rates of diabetic retinopathy progression in the UK and to define the time to progression to proliferative disease and vitreous hemorrhage in diabetic patients who present to eye care providers for the first time. They also identified the clinical features of diabetic retinopathy that are most predictive of vision-threatening disease.
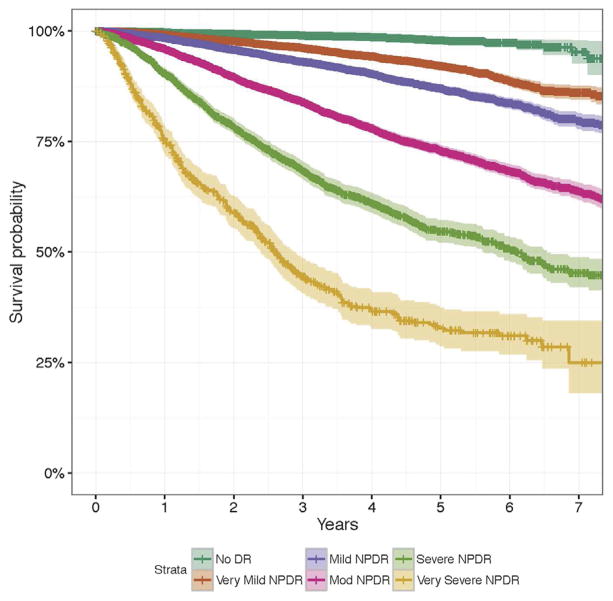
The results confirmed that baseline severity of diabetic retinopathy is predictive of patients' clinical outcomes. Approximately 44%-56% of patients with severe or very severe nonproliferative diabetic retinopathy progressed to proliferative disease or vitreous hemorrhage in less than 3 years.
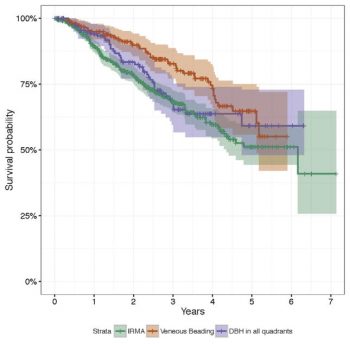
In addition, for patients with severe nonproliferative disease at baseline, the disease feature that was more predictive of progression to proliferative disease was the presence of intraretinal microvascular abnormalities. The presence of 4-quadrant dot-blot hemorrhages, however, was the most significant risk factor for vitreous hemorrhage.
One interesting consequence of these findings is that venous beading, another feature of severe disease, did not appear as critical as the other 2 features (intraretinal microvascular abnormalities and 4-quadrant dot-blot hemorrhages) in predicting proliferative diabetic retinopathy or vitreous hemorrhage. The authors note that because the latter two features can be distinguished with ocular coherence tomography, the evaluation of venous beading with or without fluorescein angiography may become less important in the future if these results are validated in other cohorts.
This study demonstrates that baseline diabetic retinopathy severities and clinical features of initial diabetic retinopathy screening remain key prognostic factors. Intraretinal microvascular abnormalities and 4-quadrant dot-blot hemorrhages are key clinical signs (which can be diagnosed on clinical examination or photography) with respect to vision-threatening disease progression, and these features should be highlighted when training staff (technicians, nurses, physicians) involved in diabetic retinopathy screening.
Lee CS, Lee AY, Baughman D, Sim D, Akelere T, Brand C, Crabb DP, Denniston AK, Downey L, Fitt A, Khan R, Mahmood S, Mandal K, Mckibbin M, Menon G, Lobo A, Kumar BV, Natha S, Varma A, Wilkinson E, Mitry D, Bailey C, Chakravarthy U, Tufail A, Egan C. The United Kingdom Diabetic Retinopathy Electronic Medical Record Users Group: Report 3: Baseline Retinopathy and Clinical Features Predict Progression of Diabetic Retinopathy. Am J Ophthalmol. 2017 Aug;180:64-71. doi: 10.1016/j.ajo.2017.05.020. Epub 2017 May 29. PubMed PMID: 28572062; PubMed Central PMCID: PMC5608549.