The use of electronic health records offers a lot of advantages in terms of providing accurate, coordinated, up-to-date care for patients and may also help to reduce medical errors. The benefits depend on widespread implementation, however, and there have been challenges with getting physicians to use electronic records because they can require extra time, effort, and cost.
To encourage physicians to implement electronic health records into their practices, an incentive program was created by the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009, which provided direct payments yearly to physicians who adopted the use of electronic health records. To earn these incentive payments, providers were expected to demonstrate meaningful use of certified EHR technology according to metrics which were linked to certain goals for the program, such as improving efficiency and coordination of care, reducing disparities, etc. The program was designed to reward early adopters, as the payments decreased after the first two years.
In this study, the authors assessed the degree to which ophthalmologists took part in this program and their continuity and success in receiving payments in comparison to other specialties. They used publicly available data sources to create subsets of payment and attestation data for ophthalmologists which were then compared to other specialties.
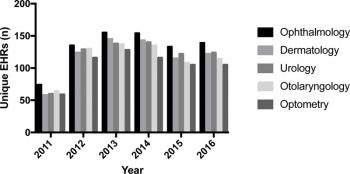
The authors found that the incentive program led to increased use of electronic health records by ophthalmologists over the life of the program. Only 6.7% of Medicare-billing ophthalmologists attested to meaningful use in the first year of the program (2011), but approximately half attested during the final four years (2013-2016). These numbers were similar to the surgical subspecialties of dermatology and otolaryngology but lower than those for urology, and all of these specialties had a higher participation rate than Medicare-billing optometrists. The percentage of payments received by ophthalmologists (3.6%) was more than twice the percentage of ophthalmologists in the population of Medicare-billing providers (1.6%).
The authors compared their findings to results from surveys about the program to help interpret the reasons practitioners chose to participate or not. The program had escalating requirements over time and many providers reported finding them burdensome. Some were concerned that the system did not improve care and/or was too expensive or otherwise challenging to implement, even when facing reimbursement penalties for not doing so.
The authors noted certain trends in the data that led them to make some interesting observations, such as how ophthalmologists may have joined the program later because they tend to use smaller electronic health vendors, who may have taken more time to get their products ready for meaningful use certification. The most commonly used electronic health record was one that is exclusively used at large health companies, suggesting that the resources required to participate in the program may favor institutions with greater economies of scale.
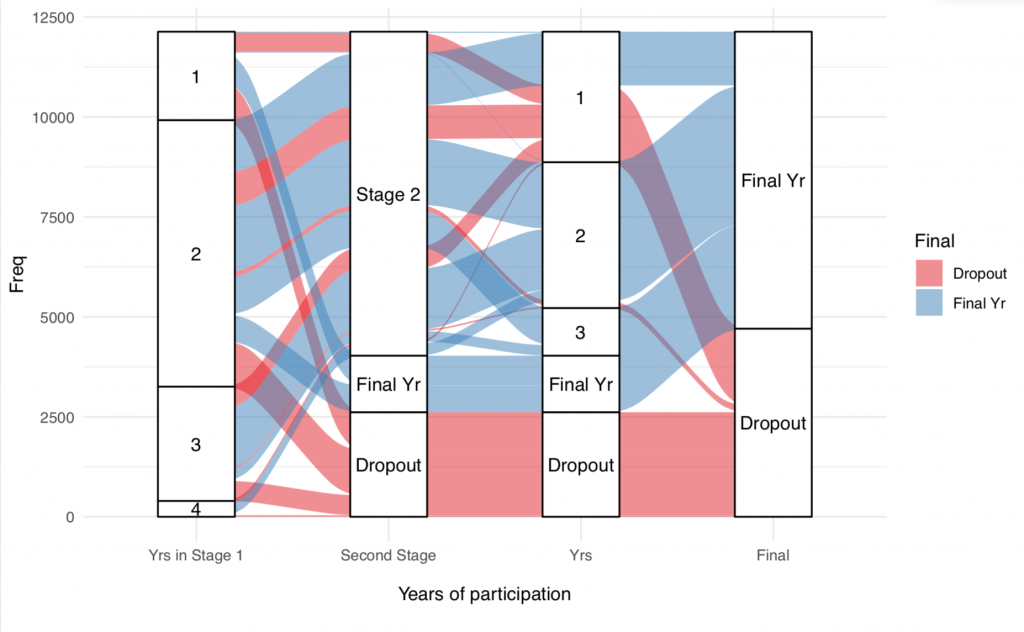
Overall, ophthalmology fared well in the meaningful use program compared to other eligible practitioners, although significant proportion did not engage at all or dropped out at some point. The authors conclude that more data is needed, particularly demographic information (type of practice, number of physicians in the practice, etc.), to help determine which factors predicted success (or failure) with the meaningful use program and to further refine the program design in order to increase participation in any future programs.
Boland MV, Hwang TS, Lim MC, Peterson JL, Lum F, Lee AY. Medicare Incentive Payments to United States Ophthalmologists for Use of Electronic Health Records: 2011-2016. Ophthalmology. 2019 Jul;126(7):928-934. doi: 10.1016/j.ophtha.2019 .01.030. Epub 2019 Feb 13. PubMed PMID: 30768941; PubMed Central PMCID: PMC6662572.